Periodontitis and rheumatoid arthritis: a common responsible
Alessandra Abbà
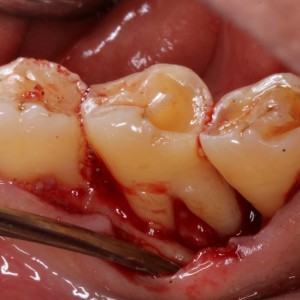
Periodontitis is a chronic inflammatory disease characterized by an irreversible loss of connective tissue attachment and alveolar bone and it is a major cause of tooth loss.
Reumatoid Arthritis (RA) is a chronic destructive multifactorial disease of unknown etiology in which genetic susceptibility, environmental and hormonal factors interact in complex ways. It’s characterized by the accumulation and persistence of an inflammatory infiltrate in the synovial membrane, resulting in synovitis and joint architecture destruction.
So what do they share?
Porphyromonas gingivalis (Pg) is a key factor in the pathogenesis both of rheumatoid arthritis (RA) and periodontitis. An increasing number of studies have demonstrated this association. Pg can induce anticyclic-citrullinated peptide autoantibodies (anti-CCP antibodies),responsible of the development of RA. Periodontitis and RA also share genetic and environmental risk factors.
In this prospective cross-sectional study, published in JPIS in 2018, authors aimed to evaluate the relationships and the clinical implications between the two diseases in Korean adults.
MATERIALS AND METHODS
The RA group included 260 patients who satisfied the 1987 American College of Rheumatology classification criteria for RA. Serologic analyses were performed for them. An age- and sex-matched control group of 86 volunteers without arthritis was enrolled too. In order to evaluate periodontal conditions, the following data were registered:
- plaque index (PI)
- gingival index (GI)
- probing pocket depth (PPD)
- bleeding on probing (BOP)
- clinical attachment level (CAL)
Periodontal indices and the prevalence and amount of periodontal pathogens were recorded and compared between the groups. Correlations between periodontal and RA indices were examined.
RESULTS
Statistacally significant higher values were registered for the RA group (P<0.05) for all periodontal indices except the number of teeth. The severity of periodontitis in all participants was slight or more than slight. The RA group showed also a significantly higher prevalence of moderate-to-severe periodontitis (64.2% vs. 34.9%, P<0.001).
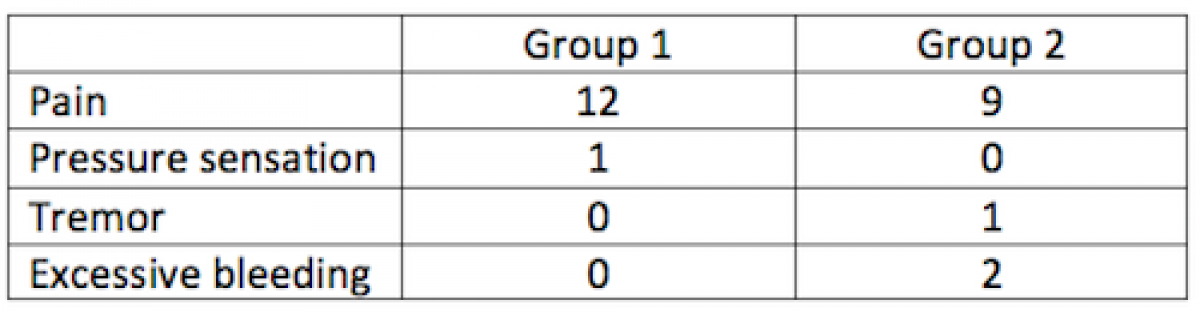
The GI, BOP, and PPD showed positive relationships with several RA indices. The anti-Pg antibody titer had positive relationships with PPD, BOP, CAL, and periodontitis severity (table 1).
CONCLUSIONS
Even if there was no significant difference in the prevalence of periodontal pathogens between the two groups, RA was associated with higher values of periodontal indices and periodontitis severity. In conclusion, alteration of periodontal indices could be used as a warning sign of disease development in RA patients and at the same time an increasing anti-Pg antibody titer could be considered as a risk indicator in RA patients suffering with periodontitis.
For additional informations:
Periodontal pathogens and the association between periodontitis and rheumatoid arthritis in Korean adults
 Related articles
Related articles
Periodontology 01 December 2025
Ceramic abutments--a new era in achieving optimal esthetics in implant dentistry.
In the visible dental region in particular, implant-prosthetic restorations filling single-tooth gaps make exacting demands on function and esthetics.
Periodontology 14 November 2025
This study was carried out to assess the oral hygiene awareness and practices amongst patients visiting the Department of Periodontology at Gian Sagar Dental College and Hospital, Ramnagar (Patiala).
Periodontology 30 October 2025
To update the competences and learning outcomes and their evaluation, educational methods and education quality assurance for the training of contemporary specialists in periodontology
Periodontology 10 October 2025
Continuous professional development (CPD) in Periodontology refers to the overall framework of opportunities that facilitate a life-long learning practice, driven by the learner-practitioner and...
Periodontology 10 September 2025
To update the findings of a systematic review from the year 2016 on the evidence for the accuracy and potential benefits of cone beam computed tomography (CBCT) in periodontal diagnostics.
 Read more
Read more
Endodontics 13 January 2026
Regenerative endodontic treatment has provided a treatment option that aims to allow root maturation.
Editorials 13 January 2026
Pitt’s New Digital Dentistry Labs to Provide State-of-the-Art Education and Patient Care
Three new dentistry labs at the University of Pittsburgh School of Dental Medicine will give students and residents hands-on experience with cutting edge digital dental technology while providing...
Products 13 January 2026
Revolutionizing Pediatric Dentistry with Dr. Josh Solomon: SDI Stela & Bioclear Insights
Join pediatric dentist Dr. Josh Solomon as he discusses the cutting-edge SDI Stela self-curing composite system and the Bioclear matrix system, and how these products are transforming Class II...
News 13 January 2026
Curve Dental, the leading cloud-native, all-in-one dental practice management platform, today announced its recognition as a market leader in The 2026 Dental Technology Landscape: Cloud, AI, and the...
News 13 January 2026
Patterson Companies Inc. has announced the appointment of Patrik Eriksson as Patterson Dental’s North American president. Eriksson brings a wealth of experience in the dental and medical technology...