Fixed metal free teeth replacement with two-piece ceramic implants: a two-year case report
Sammy Noumbissi
Introduction
Dental implants have revolutionized dentistry as well as fixed and removable prosthodontics. Although the success of titanium is undisputable, the widespread use of implants has come with problems ranging from cosmetic concerns to systemic effects on the recipient. There have been increasing reports and research on the long-term stability of titanium and titanium alloys in the oral environment. Corrosion and release of metal ions in peri-implant tissues has been proven to be an issue and has been subject to investigation in recent years. The clinical situation presented here is one where metal sensitivity was a concern.
Clinical Case
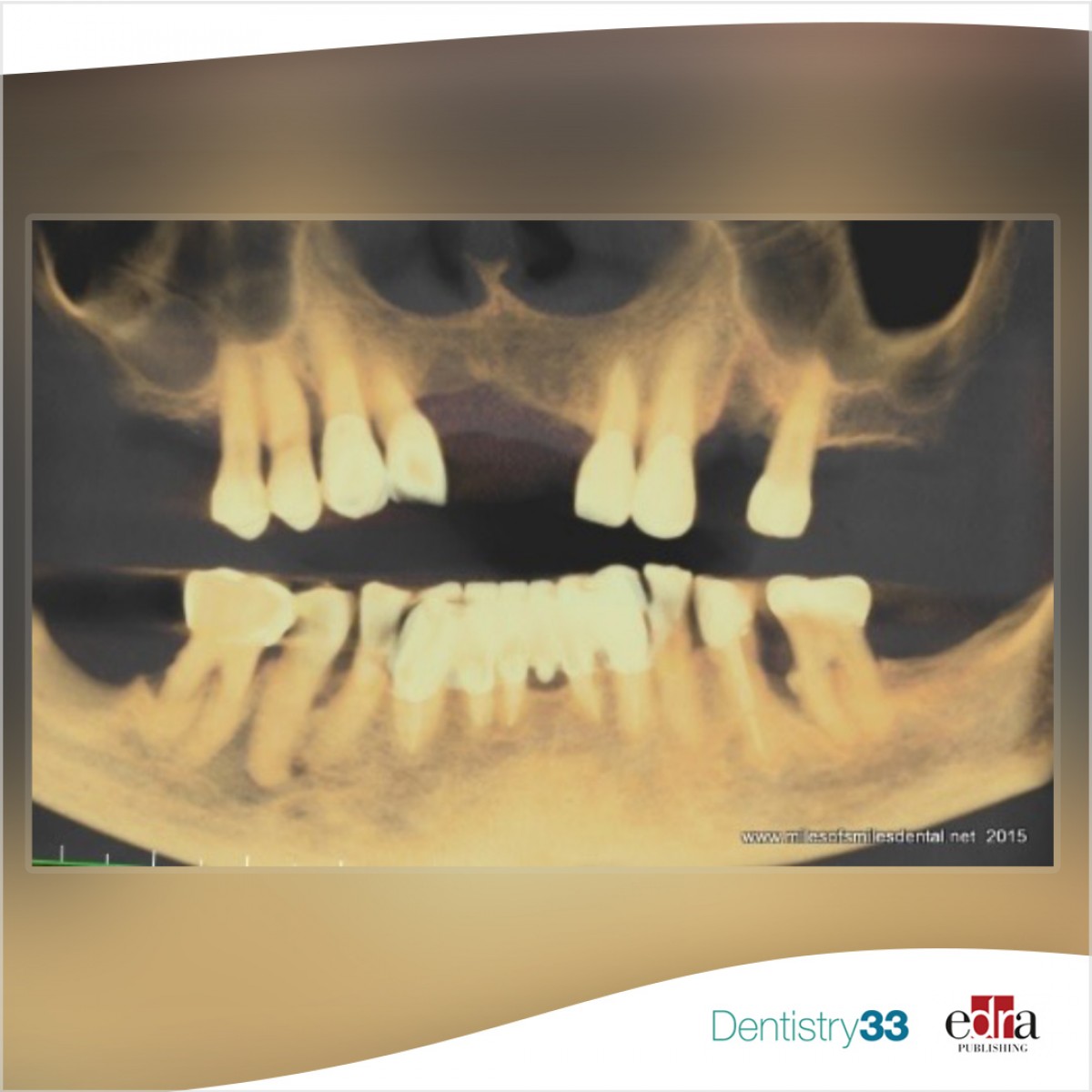
A 59-year-old male presented partially edentulous with severe collapse in the vertical dimension of occlusion. Most teeth were periodontally involved or fractured at the gingival level. The periodontally involved teeth had mobility type II with moderate to advanced bone loss and gingival recession (Figure 1, above).
Only three mandibular teeth were present with no teeth remaining in the mandibular left quadrant and moderate to advanced vertical bone loss (Figure 2). A cone beam CT scan was obtained and reviewed to assess bone levels, anatomy as well as critical anatomical structures in the areas of planned implant placement (Figure 3).
The patient had difficulty wearing removable appliances, had a severe gag reflex and wanted a metal free fixed solution to replace his teeth. Alternative treatment options were presented including overdentures on four ceramic implants. The patient opted for maxillary and mandibular fixed full arch screw-retained prosthetics using zirconia ceramic implants. A two-phased treatment plan consisting initially of full arch extractions, immediate implant placement in both arches and soft –reline immediate dentures for both arches.
The patient returned for surgery, a consent form was obtained, local anesthesia was administered across the maxillary arch by infiltration and bilateral posterior superior alveolar blocks. For the mandible anesthesia was obtained by means of cross arch local infiltration. Extractions of all remaining teeth was done atraumatically using manual periotomes and piezotome all the while taking care to preserve the buccal plate on both arches.
The patient returned for surgery, a consent form was obtained, local anesthesia was administered across the maxillary arch by infiltration and bilateral posterior superior alveolar blocks. For the mandible anesthesia was obtained by means of cross arch local infiltration. Extractions of all remaining teeth was done atraumatically using manual periotomes and piezotome all the while taking care to preserve the buccal plate on both arches.
Four months post-surgery the implants were uncovered, and the soft tissue above the implants’ cover screws was removed with a diode laser where needed. The smart pegs specifically designed for the implants were screwed into the implants and stability measurements were made using resonance frequency analysis technology. This modality has been well proven and documented to assess implant stability and biological readiness for the implants to be restored. The Ostell device (shown in Figure 7a, lower right) was used to measure the implant stability level for each implant after four months of healing time.
Four months post-surgery the implants were uncovered, and the soft tissue above the implants’ cover screws was removed with a diode laser where needed. The smart pegs specifically designed for the implants were screwed into the implants and stability measurements were made using resonance frequency analysis technology. This modality has been well proven and documented to assess implant stability and biological readiness for the implants to be restored. The Ostell device was used to measure the implant stability level for each implant after four months of healing time.
Five two-piece ceramic implants were placed in the maxilla as well as in the mandible. The manufacturer’s surgical kit and protocol was closely followed. Insertion torque value for all implants was 25 Ncm and all implants showed good initial clinical primary stability. However, one of the mandibular implants failed to osseointegrate and was removed two months after placement. The patient elected not to have it replaced with another implant.
All implants returned average Implant Stability Quotient Values (ISQ) values above 74. Given that the acceptable value range for safe loading of dental implants is between 55 and 85, it was determined that the implants were ready for loading with permanent fixed prosthetics.
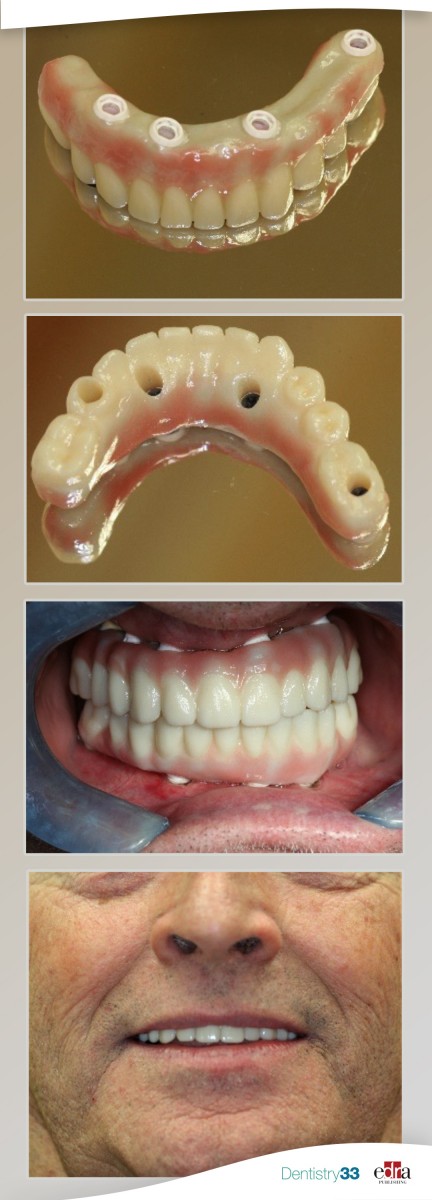
Conventional impressions were made using polyvinylsiloxane heavy and light body with the closed tray technique. The fabrication of a hybrid prosthesis was started by going through the process of making a conventional denture. Wax rims, wax try-in were done for space analysis, facial contour occlusion, phonetics and aesthetics. Once the waxed prototype was approved, multiple clinical photographs and bite registration were taken for effective transfer of information to the dental laboratory. The zirconia prosthesis framework was manufactured with CAD/CAM technology after scanning of the wax-up prosthesis. A try-in of the framework was done to verify and confirm passive fit to the implants on both arches. The frameworks were returned to the laboratory for overlay of pressed ceramic.
The screw-retained all-ceramic porcelain fused to zirconia bridge was connected to the implants, occlusion checked and adjusted where needed.
The patient was satisfied with aesthetics of the prosthetics. A soft night guard was provided to the patient.
The patient has been followed up with periodically for the last 24 months and there have been no complications to date.
Conclusion
Full mouth rehabilitation with two-piece screw-retained ceramic implants is an option. Two-piece ceramic implants are easier to transition into for a clinician familiar with conventional titanium and titanium alloyed implants. However, it should be noted that case selection and rigorous treatment planning are crucial for the success of such rehabilitations. Ceramic implants do not have the prosthetic flexibility and options their titanium counterpart have, therefore biomechanically and prosthetically driven treatment is very important.
 Related articles
Related articles
USA 08 December 2023 - 09 December 2023
Ceramic Implants: Two-day hands-on and live patient training course – December 2023
The macroscopic and microscopic differences between ceramic implants and titanium implants.
Dental materials 09 August 2023
Featured dentist: Dr. Alexandre Marques, a father, dentist, professor and student
A member of the International Academy of Ceramic Implantology, Marques was awarded third place in a poster competition at the organization’s 2023 congress.
USA 13 April 2023 - 15 April 2023
The Congress will highlight an impressive roster of expert speakers and researchers in the field of bio ceramics and metal-free implant dentistry. Lectures and workshops have been selected with the...
USA 13 April 2023 - 15 April 2023
April 13 - 15, Atlanta
This is the twelfth year for the event, which will feature some of the world’s foremost biomaterials experts, bioceramics industry leaders and experienced clinicians in the field of ceramic...
Implantology 24 March 2023
By André Zétola and Isabela Zago Zétola
The aim of this case report was to share results of a clinician installing metal-free implant associated with simultaneous GBR in anterior upper jaw. ...
 Read more
Read more
Endodontics 13 January 2026
Regenerative endodontic treatment has provided a treatment option that aims to allow root maturation.
Editorials 13 January 2026
Pitt’s New Digital Dentistry Labs to Provide State-of-the-Art Education and Patient Care
Three new dentistry labs at the University of Pittsburgh School of Dental Medicine will give students and residents hands-on experience with cutting edge digital dental technology while providing...
Products 13 January 2026
Revolutionizing Pediatric Dentistry with Dr. Josh Solomon: SDI Stela & Bioclear Insights
Join pediatric dentist Dr. Josh Solomon as he discusses the cutting-edge SDI Stela self-curing composite system and the Bioclear matrix system, and how these products are transforming Class II...
News 13 January 2026
Curve Dental, the leading cloud-native, all-in-one dental practice management platform, today announced its recognition as a market leader in The 2026 Dental Technology Landscape: Cloud, AI, and the...
News 13 January 2026
Patterson Companies Inc. has announced the appointment of Patrik Eriksson as Patterson Dental’s North American president. Eriksson brings a wealth of experience in the dental and medical technology...