The technological evolution of CBCT machines: an opportunity for modern endodontics.
Author: Dr. A. Bebi
Recent years have seen CBCT exams become increasingly widespread and, as machine development continues to expand their application range, they look set to play an ever-greater role in dentistry.
The justification principle - on which surgeries rely to guide their X-ray requests - is the most limiting factor in selecting CBCTs as first-level examinations and can, moreover, sometimes limit their use as second-level examinations. However, responsible, properly informed use of 3D radiology is essential in modern dentistry.
Ongoing development of cone beam machines is providing us with ever-better equipment, in terms of both versatility and the dose absorbed by the patient, thus expanding their scope.
An ability to master the software and an intricate understanding of setting parameters in relation to the pathology to be investigated are by far the most important factors in keeping doses effective yet as low as possible. Frequently, we've seen dentists use an FOV (Field Of View) that is too large for the anatomical area of interest, or resolutions inadequately calibrated for the problem under investigation. A dentist who, for example, needs to analyse the three-dimensional position of a tooth embedded in the bone and its relationships with teeth adjacent to it, would gain no benefit from a 13x16 FOV or a high resolution. On the other hand, a search for a root fracture or assessment of anatomical difficulties prior to endodontic retreatment will benefit greatly from the highest possible resolution and an FOV that ideally includes only the tooth in question.
This lengthy introduction, then, leads us to an illustration of our own experiences with a new CBCT unit; its use has allowed us to significantly improve some clinical procedures, making them simpler and more predictable.
The machine in question is a Hyperion X9 Pro characterised by a broad range of FOVs, which extend from 13x16 to 6x6 - with plenty of intermediate steps - and up to 4x4 at 68 microns when equipped with the optional XF (eXtended Functions) package. Moreover, this same machine lets users select one of three different resolutions for each examination: ‘quick’, ‘regular’ and ‘best quality’. These protocols are specifically designed to provide the most suitable response to various clinical situations such as control exams (Quick), basic diagnostics (Regular) and investigations into micro-pathologies such as micro-fractures or secondary canal searches (Best Quality).
Maximum resolution is 68 microns, allowing us to observe details that are not as clearly visible at lower resolutions.
The purpose of this paper is to assess, via the presentation of three case studies, whether the ability to increase the resolution of the above-cited machine to 68 microns constitutes a significant, advantageous opportunity in the dentist's daily clinical practice.
First case: 58-year-old female patient, colleague.
After having incurred a 3.5 root fracture with considerable loss of vestibular bone, it was decided that treatment should involve extraction of the coronal fragment and application of an endocanalar pin for "slow" orthodontic extrusion mechanics in order to recover bone tissue. Extraction of the tooth in its entirety and construction of a prosthetic implant followed.
After a few months of orthodontic treatment, a couple of fistulization episodes - which seemed to come clinically from zones 3.5 and 3.6 - led us to make new diagnostic investigations.
A high-resolution 4x4 CBCT was therefore performed to search for further presumable fractures and assess the quantity of regenerated bone.
Unfortunately, the cross-sections highlighted the presence of a further fracture, again in 3.5, which at this point suggested immediate extraction. It's interesting to note that the evidently vestibular position of the lesion would have made it invisible in any 2D examination (fig. 1).
In this case, though, identification of the fracture meant we were able to interrupt a treatment plan that would have failed to yield the desired results. Infection-related vestibular bone resorption along the fracture line would, in fact, have occurred faster than the regeneration obtained with the orthodontics.
Second case: female patient, 45 years old
This patient came to us with purulent swelling in zone 2.6. Moreover, she informed us that the tooth had been devitalized in childhood and that, a few years earlier, when a CBCT had been performed at our surgery for implant reasons, an attempt at root canal treatment had been recommended due to the presence of an apical rarefaction.
Since, over the years, the patient had never experienced any discomfort, and since successful root canal treatment could not be guaranteed, she had not consented to endodontic treatment.
An intraoral X-ray revealed a clearly short root canal filling and a periapical radio-transparency of considerable size in zone 2.6 (Fig. 2).
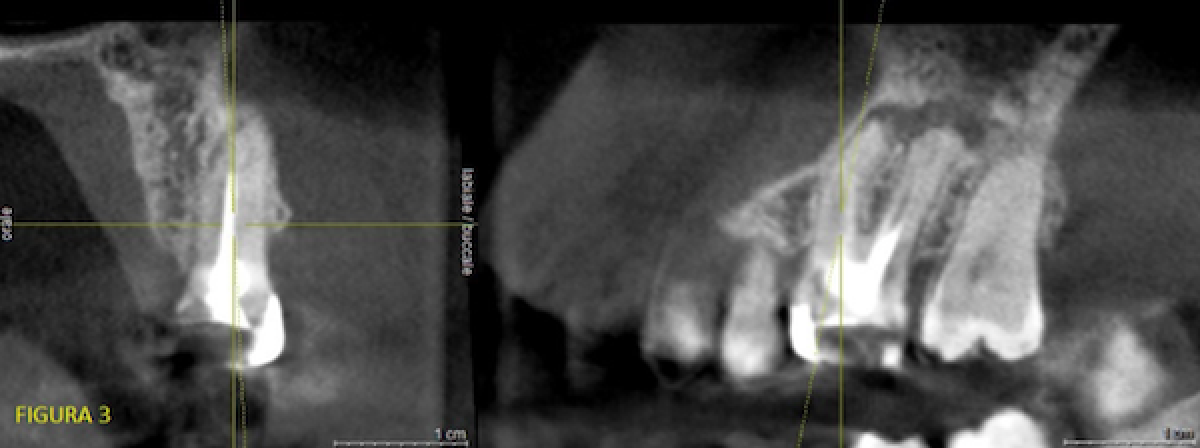
After observing the CBCT performed 4 years earlier at a resolution of about 100 microns, we were able to state that the apical radio-transparency, while present, was smaller and that, unfortunately, it was impossible to obtain endodontic morphology information useful for facilitating treatment (Fig. 3).
Stating first that I am a general dentist, and that an endodontic specialist with an expert eye would probably have been able to respond on the basis of a simple X-ray and perhaps also proceed successfully with therapy without further tests, we decided on a 'best quality' 4x4 CBCT (high resolution) to investigate the case further.
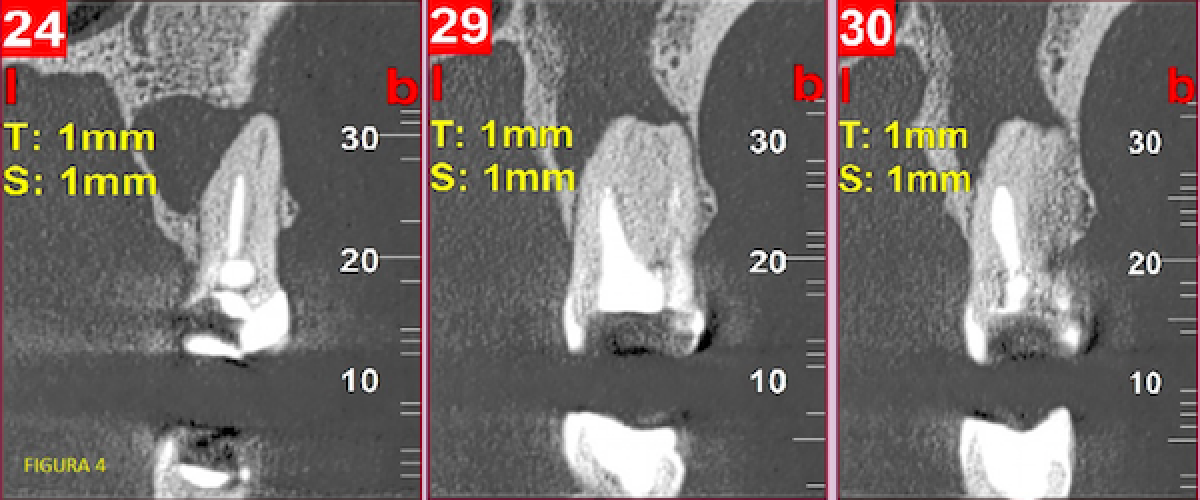
This examination revealed the presence and patency of a second canal on the mesiovestibular root; it also revealed its position and starting point. Said canal reached the root apex much more apically than the already-treated canal which, however, could no longer be probed (fig. 4).
The entrance to the unprobed canal was radiologically obstructed by just 1-2 tenths of a millimetre. The relationship with the already-treated canal, together with the relative coronal position of the entrance, reassured us as to the possibility of probing it.
We therefore approached retreatment without the aid of an occlusal tracking template (we sometimes use the latter in cases where the canal is sclerotic for an extensive coronal tract before becoming patent again).
The other two canals, the palatal and distovestibular, were radiologically sclerotic for a brief tract apically at the terminus of the canal filling and then clearly visible again up to the anatomical apex.
Their careful examination made finding the untreated canal much easier, minimising the risk of iatrogenic damage.
Such damage could have occurred in an insistent attempt either to probe the mesiopalatal canal more apically or to search for the entrance to a possible mesiovestibular canal without having prior knowledge of its existence or position.
Instead, being able to analyse the X-ray image of patent endodontic spaces apically to the pre-existing root canal filling encouraged us to carry on probing beyond the working length previously reached by the colleague.
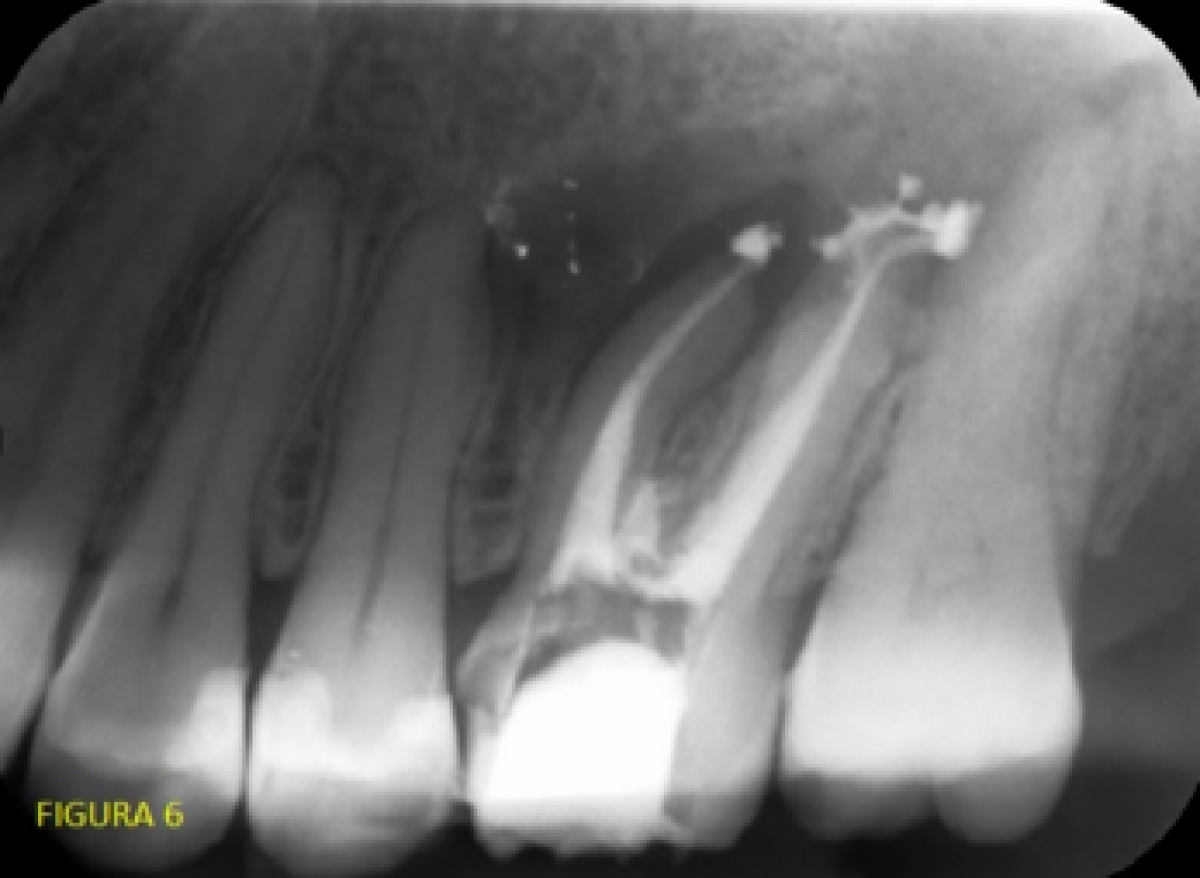
This meant we were able to retrace the canals in question and reach the apexes (even going a little beyond them with the cement). See end-of-treatment control X-ray (fig. 6).
Third case: female patient aged 35
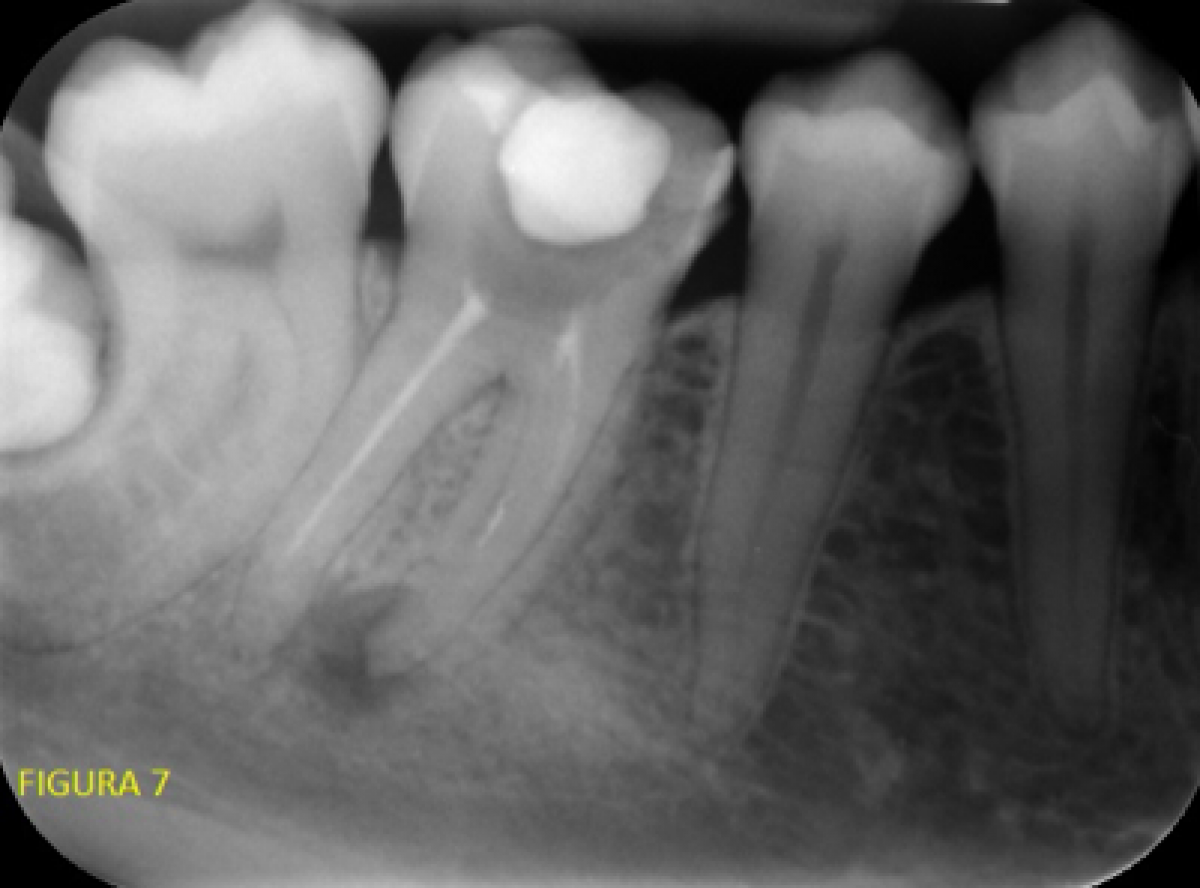
The patient came to us with painful symptoms on percussion and with increased mobility at 3.6. As a first-level analysis, we performed an intraoral X-ray with the Rinn alignment system.
Highlighted features included an area of radio-transparency on the mesial root of zone 3.6, no alterations on the apex of the distal root, earlier root canal treatment evidently short on both roots.
Again, in this case we resorted to preventive assistance by way of a second-level examination, running a 4x4 volume on the tooth in question at maximum resolution with the Hyperion X9 Pro.
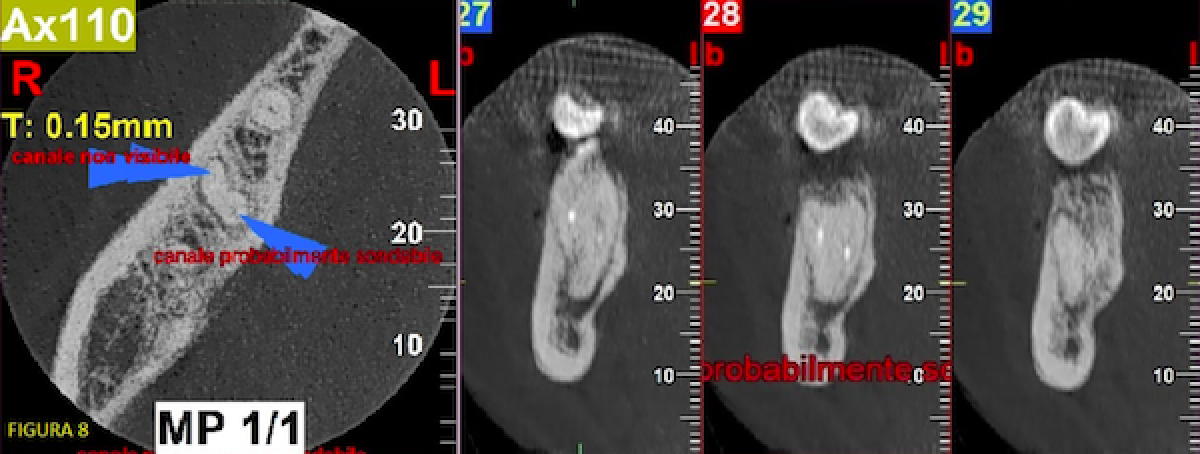
Extensive, expert use of the software highlighted the presence of a patent canal as far as the apex in the medial root with a small radio-opaque area that could not be identified (broken instrument? cement?). Nevertheless, the possibility of being able to overcome the obstacle could be glimpsed.
The other two canals were not apically detectable at the end of the existing root canal fillings (fig. 8).
We proceeded with treatment of 3.6 by intervening with instruments on the radiologically viable mesio-lingual canal up to the anatomical apex.
In the other two we insisted relatively little in trying to get to the apex, deeming it easier to create a false path than go through a canal so small as to be undetectable with a 68-micron CBCT examination. Intraoral X-ray at the end of retreatment (fig. 9).
Conclusions
Sharing our clinical experience of using different CBCT machines and their software will, we believe, prove helpful to colleagues and allow them to assess, with greater awareness, what can be obtained from these different machine types from both a purchasing standpoint and as regards requesting examinations from radiological institutes.
In our opinion, the dentist's mastery of the software, together with a choice of FOV and examination resolution that are suitable for the clinical problem being addressed, are by far the most important factors in the biological costs-clinical benefits ratio (ALARA principle).
Cutting-edge, high performance devices such as the Hyperion X9 Pro used in these case studies constitute a significant step forward when it comes to seeing the fundamental details that guide a dentist's approach to treatment.
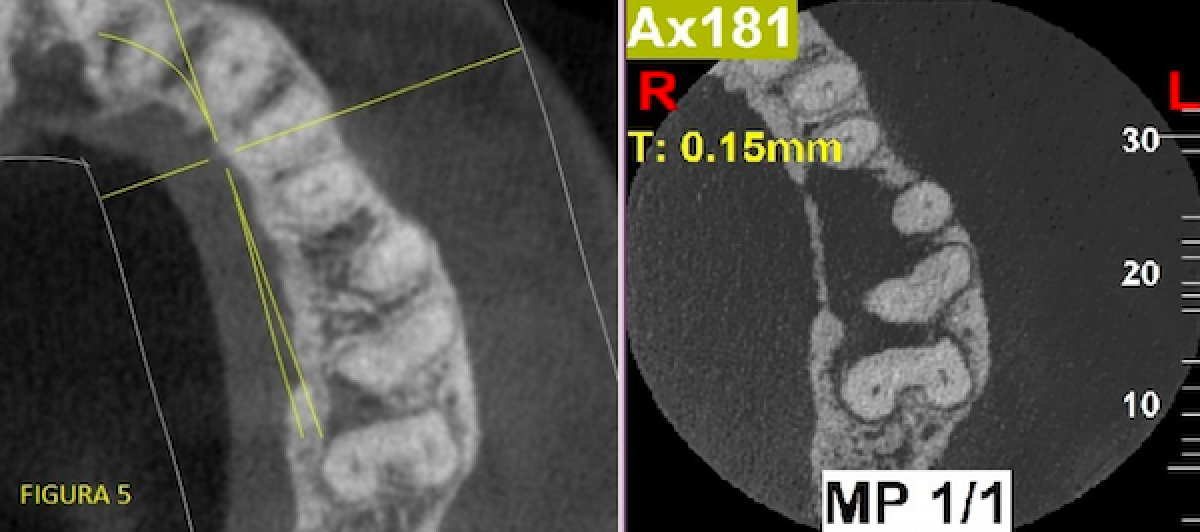
Ultimately, these machines provide accurate, measurable information by rendering visible what remains invisible with lower resolution machines. Compare with Fig. 5.
Another feature of latest-generation CBCTs is versatility. They let users perform the same exams that used to be done with the first models and the higher resolution ones used in these case studies. Additional uses - which we greatly appreciate - include the ability to use small and very small FOVs at low resolution, making them examinations that satisfy the justification principle in cases where we would be uncomfortable with higher doses.
In conclusion, new CBCT units such as the Hyperion X9 Pro constitute excellent dentistry tools. Lastly, their broadened scope obliges us to lengthen our learning curve so we can use them to their full potential and do so more responsibly.
 Related articles
Related articles
USA 22 February 2024 - 24 February 2024
Early-bird rates available through Nov. 30
The 2024 Midwinter Meeting provides exceptional continuing education featuring top dental speakers, an expansive Exhibit Hall with the best vendors in the country and opportunities to meet old and...
News 06 February 2024
Carestream Dental is providing oral healthcare professionals a seamless transition to CBCT imaging with the CS 8200 3D Access.
Endodontics 29 August 2023
Effect of field of view, voxel size on CBCT accuracy of navigation in endodontic microsurgery
This study aimed to evaluate the influence of field of view and voxel size on the accuracy of dynamic navigation–assisted endodontic microsurgery.
Endodontics 25 August 2023
CBCT segmentation, additive manufacturing for management of root canals with ledges
CBCT assessment of a ledge could be useful to a clinician, however, utilizing this information effectively during a treatment procedure can be challenging.
Doctors will now have even greater flexibility with the introduction of Spark Approver Web and seamless DEXIS IOS integration, along with exciting clinical and workflow updates.
 Read more
Read more
Editorials 16 April 2024
Dr. Kyle Vining Earns Hartwell Foundation Award to Study Childhood Leukemia
Every year, thousands of American children are diagnosed with acute lymphoblastic leukemia (ALL), the most common form of childhood cancer. The disease begins in bone marrow, when immature cells...
News 16 April 2024
The UF College of Dentistry notched a record turnout for its annual celebration of research – Spring Synergy – on Friday, March 29 at the HPNP Auditorium
Products 16 April 2024
Glidewell recently announced a rebrand of its flagship Hahn Tapered Implant System, now known as the Glidewell HT Implant System.
Market 16 April 2024
Zentist Launches Cavi AR, an RCM Software for Dental Insurance AR & Claims Management
Zentist, the leading cloud-based insurance Revenue Cycle Management (RCM) software for U.S. dental groups, proudly announces the introduction of Cavi AR, an additional innovative solution that is...
News 16 April 2024
Standard Dental Labs Sets Sights on Expansion Following Strong FYE 2023 Performance
Costas, Inc., operating as Standard Dental Labs Inc., a renowned name in the dental industry, is pleased to announce the filing of its annual report for the fiscal year ending 2023 on April 10th,...