Periapical radiographs vs cone beam imaging in endodontic microsurgery
Lara Figini
Object of the study
Persistent apical periodontitis occurs in 14% to 39% of cases and the clinical decision-making process for choosing the relevant treatment is a challenging process that requires evidence-based information, patient-specific analyses and preferences.
Endodontic microsurgery is an effective treatment strategy when orthograde retreatment fails or is technically not feasible. Surgical planning must take into account several factors, including cortical bone thickness, root inclination and adjacent anatomical structures to reduce post-surgical complications. These include pain and swelling, hemorrhage, sinus perforation, lockjaw and difficulty chewing. The likelihood of impaired sensation after periapical surgery is significant, around 14%, with a 30% higher incidence in the premolars than in the molars (Mainkar et al., 2020).
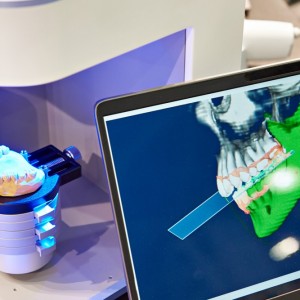
Endodontic treatment planning is influenced by radiographic information, which can contribute to a better predictable outcome. Although it is the preferred diagnostic imaging method, “noise” and anatomical overlay can hamper the data obtained from periapical radiographs (PR), resulting in a narrow two-dimensional field of view. On the other hand, CBCT images provide information in three orthogonal planes and can provide additional data on root inclination, precise extent of the periapical lesion and its spatial relationship with anatomical structures, thickness and status of the cortical plate for preoperative planning of multi-rooted teeth undergoing periapical surgery.
Type of research and methods of analysis
In a parallel group randomized controlled study published in the International Endodontics Journal in January 2023, the authors evaluated whether the use of additional cone beam computed tomography (CBCT) imaging could have positive effects on quality of life and healing outcome after periapical surgery versus periapical radiographs (PR) alone.
Researchers assigned 52 patients with persistent apical periodontitis and radiographic evidence of periapical lesion to the PR or CBCT group. The main predictor of the study was the type of imaging method, PR alone or with additional CBCT.
The primary outcome investigated was the patient's quality of life during the first week after periapical surgery and secondary outcomes investigated were the duration of surgery and healing outcome at the 12-month follow-up. Participants in both groups received periapical surgery based on the pre-surgical plan provided by pre-specified radiographic imaging methods. Quality of life (QoL) was assessed using the modified Shugars questionnaire. Radiographic analysis for healing of periapical lesions was conducted using Molven criteria and modified PENN 3D criteria. Between-group categorical data were analyzed using the Chi-square test, while intra-group comparisons were analyzed using the McNemar test. Mean scores for each component of QoL (oral function, general function, pain, swelling, and others), combined QoL scores (overall mean of the values of 13 variables), and analgesic intake each day were calculated and analysed.
Results
At a 12-month follow-up, the team evaluated 50 patients. Participants in the PR group reported significantly more swelling in the first three days than those in the CBCT group. Analgesic intake was higher in the PR group on day two and day three (Mann–Whitney U test with Bonferroni correction; p<.007).
The research team observed a significant difference in the limitation of general functions on the second day with the highest values in the PR group. The combined QoL score between the two groups was not significant. However, none of the patients had intraoperative complications or neurovascular damage. Mean surgical time was shorter in the CBCT group. Radiographic healing revealed a success rate of 96.2% for the PR group and 95.8% for the CBCT group with no significant differences between groups.
Conclusions
From the data of this study, researchers concluded that the use of CBCT in endodontic microsurgery substantially guarantees fewer complications such as early postoperative swelling and limitations of general functions. However, preoperative CBCT has no effect on other investigated QoL parameters and intraoperative complications in medium-risk patients. Furthermore, CBCT has no additional advantage over periapical radiography in terms of evaluating the healing outcome after endodontic microsurgery. CBCT offers surgically relevant anatomical information for pre-surgical planning and to ensure treatment yield with significantly reduced operative time.
Clinical implications
Strengths of this study include the previous sample size estimate, a single operator who performed all the procedures and the correct procedure blinded by the evaluators. Motivation for using CBCT also complied with AAE/AAOMR recommendations. However, the study has some limitations which include a small number of posterior teeth and mandibular anterior teeth. Use of the Likert rating scale to assess QoL and postoperative pain is subjective, with the possibility of bias.
Future long-term studies with a larger sample size focusing on targeted surgical approaches in patients at high risk for neurovascular injury are needed for a better understanding of the impact of preoperative imaging on periapical surgery outcomes.
Mainkar, A., Zhu, Q. & Safavi, K. "Incidence of altered sensation after mandibular premolar and molar periapical surgery." (2020) Journal of Endodontics. 46, 29–33. DOI: 10.1016/j.joen.2019.10.008
Keerthana Gurusamy, Jigyasa Duhan, Sanjay Tewari, Pankaj Sangwan, Ambika Gupta, Shweta Mittal, Vinay Kumar, Mayank Arora. "Patient-centric outcome assessment of endodontic microsurgery using periapical radiography versus cone beam computed tomography: A randomized clinical trial." Int Endod J. Jan 2023; 56:3–16. DOI: 10.1111/iej.13837
 Tag
Tag
 Related articles
Related articles
Periodontology 10 September 2025
To update the findings of a systematic review from the year 2016 on the evidence for the accuracy and potential benefits of cone beam computed tomography (CBCT) in periodontal diagnostics.
Orthodontics 02 April 2025
CBCT in orthodontics: assessment of treatment outcomes and indications for its use
Since its introduction into dentistry in 1998, CBCT has become increasingly utilized for orthodontic diagnosis, treatment planning and research.
The use of cone beam computed tomography (CBCT) in the diagnosis and/or management of endodontic problems is increasing and is reflected in the exponential rise in publications on this topic in the...
Oral surgery 27 September 2023
Alveolar bone morphologic predictors for guided bone regeneration in anterior maxilla
This study aimed to explore the influence of alveolar bone morphologic variables on the outcome of guided bone regeneration in the anterior maxilla region.
 Read more
Read more
Much like EMTs rushing to the scene after an accident, stem cells hurry to the site of a skull fracture to start mending the damage. A new finding has uncovered the signaling mechanism that triggers...
Products 05 November 2025
SimplyTest has launched a groundbreaking saliva-based test to detect high-risk strains of oral human papillomavirus (HPV), a major cause of oropharyngeal cancers.
News 05 November 2025
Perimetrics, Inc., a dental technology company pioneering quantitative diagnostics, announced today that the U.S. Food and Drug Administration (FDA) has granted clearance for the InnerView...
News 05 November 2025
On October 15, open enrollment for Medicare began nationwide. Hundreds of thousands of seniors in New Jersey will once again face the challenge of finding the right Medicare coverage, including the...
Digital Dentistry 04 November 2025
Digitalisation is an expanding field in dentistry and implementation of digital teaching methods in dental education is an essential part of modern education.