Dr. Nick Fahey: ‘My book is a love letter to guided surgery’ Part II
Mary Guiden
In this second part of a two-part interview, Dr. Nicholas Fahey talks about his new book that offers practical applications and solutions for simplifying dental implant cases. He is a specialist in prosthodontics and an expert in all aspects of implant dentistry, practicing in Woodborough House, located in Berkshire in Southeast England.
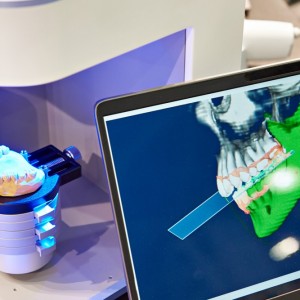
“Guided Surgery: Making Implant Placement Simpler” provides an overview of virtual surgical planning, offering a path for clinicians to learn more about the fascinating world of computer guided implant surgery. Fahey is the lead clinician for a team that practices a multidisciplinary approach to patient treatment and care. He is involved in all aspects of digital dentistry, in particular, using CBCT scans in conjunction with virtual implant planning software for computer-guided surgery. Also, more recently, Fahey has become interested in guided surgical navigation, 3D facial scanning and digital analysis of jaw movement in real-time using MODJAW. He has lectured worldwide on topics such as computer-guided surgery and virtual implant planning.
 Related articles
Related articles
Digital Dentistry 04 November 2025
Digitalisation is an expanding field in dentistry and implementation of digital teaching methods in dental education is an essential part of modern education.
News 03 November 2025
Dandy, a fully digital dental lab, today unveiled two new products for digital dentistry: the revolutionary Dandy Vision intraoral scanner and the powerful.
Editorials 02 October 2025
U-M School of Dentistry hosts national symposium on digital dentistry education
The University of Michigan School of Dentistry hosted a national Digital Dentistry Educators Symposium last week that drew faculty and leaders from 35 dental schools around the country.
Digital Dentistry 29 August 2025
Digital dentistry: The new state of the art — Is it disruptive or destructive?
Summarizing the new state of the art of digital dentistry, opens exploration of the type and extent of innovations and technological advances that have impacted – and improved – dentistry.
Endodontics 15 August 2025
Feasibility of Implementing Digital Dentistry Section in Dental Clinic of a Military Centre
Digital dentistry is not the wave of the future, it is happening now. Whether a dentist embraces the new technology determines the quality of treatment and possibly his future; for this reason,...
 Read more
Read more
Prosthodontics 17 November 2025
The purpose of this report is to describe a new technique to fabricate and deliver an implant-supported fixed prosthesis to the patient on the day of surgery, and to propose a protocol for the...
Editorials 17 November 2025
The Langkamp Allison Award recognizes a Pitt Dental Medicine third-year dental student interested in pursuing a career in dental education.
Products 17 November 2025
VELMENI today unveiled VELMENI Voice, an AI-driven voice recognition tool designed to transform periodontal charting and clinical documentation.
News 17 November 2025
Angelalign Technology Inc. (6699.HK) (“Angel”) recently announced the expansion of its flexible iOrtho platform to include direct integration with the Dexis, Shining 3D, and Panda scanners.
News 17 November 2025
Following the first FDA clearance for technology that measures internal mobility in teeth, Perimetrics CEO and Chairman Robert Hayman is once again leading dentistry into a new era with InnerView, a...