Connection between Adverse Pregnancy Outcomes and Periodontal Disease
Edoardo Mancuso
It is well known that during pregnancy, significant fluctuations in the levels of female sex hormones take place. Progesterone and estrogen reach peak plasma levels that are 10 and 30 times, respectively, higher than those observed during the menstrual cycle.
The temporary elevation of these sex hormones throughout gestation has been correlated with an increase in the prevalence, extent, and severity of gingival inflammation. In fact, receptors for these hormones have been identified in various periodontal cell subsets, rendering periodontal tissues a possible target for this high level hormonal presence.
This type of hormonal driven gingivitis is very similar to plaque‐induced gingivitis, with the exception that there is an overt severity of gingival inflammation in the presence of relatively low amounts of plaque. In particular the severity of the gingival inflammation is accentuated during the second and third gestational months without concomitant changes in plaque index.
However the main role played by female sex hormones, especially progesterone, is to regulate several vital processes during gestation, such as embryo implantation, maintenance of gravidity, gestational immune responses, induction of parturition, and cervical ripening. It is hence obvious, that any triggering mechanisms that may disturb these physiologically complex processes may contribute to the development adverse pregnancy outcomes, including mainly preeclampsia, intrauterine infections, preterm birth, low birth weight, spontaneous miscarriage, and/or stillbirth.
Therefore considering the relatively high incidence of periodontal disease, and especially of gingivitis, among pregnant women, and that the periodontal disease is both preventable and treatable, this potential association with adverse pregnancy outcomes becomes extremely important for health care providers.
A recent review written by Professor Bobetsis and his team, published on Periodontology2000, aimed to evaluate the available evidence regarding the possible association of periodontal disease with adverse pregnancy outcomes.
In the review, Bobetsis explains that during pregnancy, the elevated levels of female sex hormones increase vascular permeability and that in combination with the gingival inflammation and bleeding induced by periodontal infection may enhance the leakage of periodontal pathogens from the infected periodontal tissues to the blood circulation. This hematogenous dissemination of commensal and pathogenic microbes could enable the establishment of a metastatic infection at the feto-placental unit.
The article continues assessing that, also inflammatory mediators may be connected with adverse pregnancy outcomes. In fact, increased production of inflammatory mediators of periodontal origin may initiate a secondary reaction, a metastatic inflammation at the fetal-placental unit. Indeed, periodontitis-related prostaglandin E2 may contribute to the enhanced prostaglandin levels in the chorion, which in turn induces cervical ripening and uterine contraction and eventually leads to an increased risk for preterm birth.
The majority of the randomized controlled trials analyzed in the review have revealed no significant effect of nonsurgical periodontal therapy in any of the adverse pregnancy outcomes evaluated. However, criticism has emerged in the literature, since this type of intervention did not always manage to reduce periodontal inflammation to acceptable levels compatible with periodontal health.
From the literature analysis presented in the article, promising results are emerged form less aggressive treatment modalities that do not include scaling and root planning such as only using plaque-control regimens. Moreover the authors suggest that the reduction of the induced bacteremia during these interventions and their relative ease render these protocols appealing.
The article ends assessing that mechanistic studies provide strong evidence that periodontal pathogens can translocate from periodontal tissues to the feto-placental unit and initiate a metastatic infection. However, the extent and mechanisms by which metastatic inflammation and injury contribute to adverse pregnancy outcomes are still unclear and also, placental and fetal challenge by periodontal pathogens may be exacerbated by certain host immune response profiles, analogous to those seen in aggressive periodontitis. The majority of high‐quality randomized controlled trials analysed in the review revealed that nonsurgical periodontal therapy during the second trimester of gestation is safe but does not affect pregnancy outcomes.
In conclusion it is to point out that maternal periodontal therapy is safe for both the mother and the unborn child and although it may not alter pregnancy outcomes, it improves oral health and therefore advances general health and risk factor control and enhances health‐promoting behaviors.
For additional information: Periodontal disease and adverse pregnancy outcomes
 Read more
Read more
Much like EMTs rushing to the scene after an accident, stem cells hurry to the site of a skull fracture to start mending the damage. A new finding has uncovered the signaling mechanism that triggers...
Products 05 November 2025
SimplyTest has launched a groundbreaking saliva-based test to detect high-risk strains of oral human papillomavirus (HPV), a major cause of oropharyngeal cancers.
News 05 November 2025
Perimetrics, Inc., a dental technology company pioneering quantitative diagnostics, announced today that the U.S. Food and Drug Administration (FDA) has granted clearance for the InnerView...
News 05 November 2025
On October 15, open enrollment for Medicare began nationwide. Hundreds of thousands of seniors in New Jersey will once again face the challenge of finding the right Medicare coverage, including the...
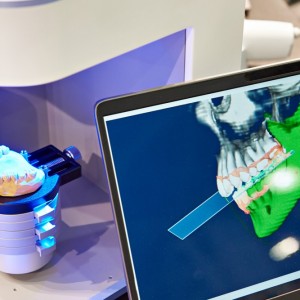
Digital Dentistry 04 November 2025
Digitalisation is an expanding field in dentistry and implementation of digital teaching methods in dental education is an essential part of modern education.