Use MRI to perform differential diagnosis between cysts and granuloma: yes or no?
Simona Chirico
Apical periodontitis is one of the most frequently problems found in endodontics. It is distinguished in its acute or chronic form. The acute form or abscess is characterized by the accumulation of polymorphonuclear neutrophils and is clinically accompanied by pain, swelling, inflammation. The chronic form can be characterized either by the granuloma or by the cyst. Granuloma has a well-developed fibrous capsule infiltrated by lymphocytes, plasma cells and macrophages. Instead the cyst can be distinguished in bay or pocket cyst when the epithelium-lined cavity is contiguous with the apex of the infected tooth; true cyst when the cyst has a cavity totally lined by epithelium and without communication with the apex.
Even if the histopathological response is considered the gold standard to differentiate a cystic from a non-cystic lesion, the diagnosis can only be performed after surgery. For this reason, we use radiological examination to identify these lesions. At the endoral radiological examination these lesions all appear radiolucent and it is not possible to differentiate them or establish the relationships they have with adjacent tissues and with the tooth itself, because they are two-dimensional images. Therefore we rely on Multislice computed tomography (CT) imaging. The problem is that this exam requires a large amount of ionizing radiation.
So Why don’t we use magnetic resonance imaging? It is non-invasive and can provide information on the structure of a lesion and its vascular components. In the study conduct by Lizio et al. they investigate the diagnostic reliability and accuracy of magnetic resonance imaging (MRI) to differentiate periapical lesions of endodontic origin and to compare the results with histopathological information.
MATERIALS AND METHODS
The radiolucent periapical jaw lesions of 34 patients, which were surgically enucleated, were investigated by two radiologists using MRI, based on the same six criteria, to categorize the lesions as granulomas, radicular cysts or others. After apicoectomies, two oral pathologists (blinded to the radiologist’s diagnoses) analysed all specimens by referring to seven specific parameters and diagnosed the specimens as granulomas, radicular cysts or other conditions. The inter-rater agreements between the radiologists and pathologists in terms of MRI and histological diagnose, respectively, along with the discriminant power of the adopted criteria and the accuracy of the MRI assessments compared with the histopathological results, were calculated. Cohen’s kappa test was adopted to examine inter-rater agreement between the two radiologists and two pathologists. Guttman’s lambda coefficient (k6) was used to evaluate the internal consistency of the items used for the differential diagnosis by radiologists. The accuracy resulted from a receiver operator characteristic (ROC) analysis.
RESULTS
A strong inter-rater reliability was observed between the two radiologists (k-statistic= 0.86, P= 0.0001) and the two pathologists (k-statistic= 0.88, P= 0.0001). The internal consistency of the diagnostic items was 0.605 for cysts and 0.771 for granulomas. The accuracy (true positives plus true negatives) of the radiologists was greater than that of the pathologists based on analysis (area under the curve= 0.87 and 0.91, respectively).
CONCLUSIONS
This trial demonstrates the reliability and accuracy of MRI as a non-invasive, pre-treatment diagnostic method for differential diagnosis between cysts and granulomas. In future, this technology should be used to verify the efficacy of root canal treatment.
For additional informations:
Differential diagnosis between a granuloma and radicular cyst: effectiveness of magnetic resonance imaging
 Related articles
Related articles
Endodontics 02 February 2026
Endodontics 23 December 2025
Serious consequences of endodontics phlegmons and abscesses of the neck: a retrospective study
In the last years there has been an alarming increase in number of patients admitted to the emergency room (E.R.) with the diagnosis of neck abscesses and phlegmons of odontogenic origin requiring...
Endodontics 08 December 2025
Evolution of Endodontics Innovations in Instrumentation, Irrigation and Filling
Endodontic treatment underwent a remarkable evolution from its beginnings, moving from rudimentary and painful techniques in the 18th and 19th centuries to advanced and specialised procedures in the...
Orthodontics 27 November 2025
Endodontically treated teeth may be moved, as endodontic treatment is not a contraindication for orthodontic treatment.
Oral surgery 26 November 2025
An apicectomy is an endodontic surgical procedure which involves root-end resection, apical curettage and root-end filling.
 Read more
Read more
Implantology 03 February 2026
Bone Structure, Metabolism, and Physiology Its Impact on Dental Implantology
When placing implants in the mandible or maxilla, it is important for clinicians to understand the process of bone remodeling, the different types of bone, and how these factors can affect the...
Editorials 03 February 2026
Dr. Alireza Sadr of the Department of Restorative Dentistry has been appointed as the first-ever UW School of Dentistry Director of Digital Dentistry and Innovation, effective Jan. 1, 2026.
Products 03 February 2026
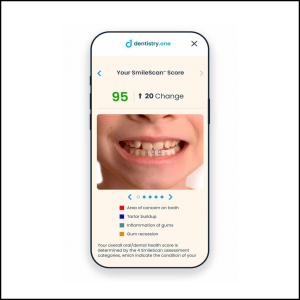
Families can now use SmileScan™, a free, AI-powered oral health scan offered by Dentistry.One, to identify potential areas of concern and receive an overall oral health score.
Investment supports professional growth for future oral health leaders and expands community outreach for underserved Oklahomans
News 03 February 2026
Henry Schein, Inc. (Nasdaq: HSIC), the world’s largest provider of health care solutions to office-based dental and medical practitioners, announced recently that it will release its fourth quarter...