Socket sealing post-extractive with xenogenic porcine collagen matrix: a prospective clinical trial
Co-authors: A. L. Rossi, V. Capilupi, D. Palombo - Department of biomedical, surgical and dental sciences, Università degli studi di Milano, ASST Santi Paolo e Carlo, Clinical Unit of Oral Surgery
Matteo Chiapasco
INTRODUCTION
Tooth extraction is associated with a significant alteration of the soft tissues surrounding the post-extraction alveolus. The alveolar bone crest preservation techniques are used in clinical practice to reduce the volumetric bone contraction that occurs as a result of the avulsion of a dental element and, at the same time, to restore the correct profile of hard and soft tissues. Within these techniques, different research activities have focused on the development of new materials and new surgical techniques, useful for the increase and preservation of the keratinized mucous tissue positioned around the rehabilitations on implants.
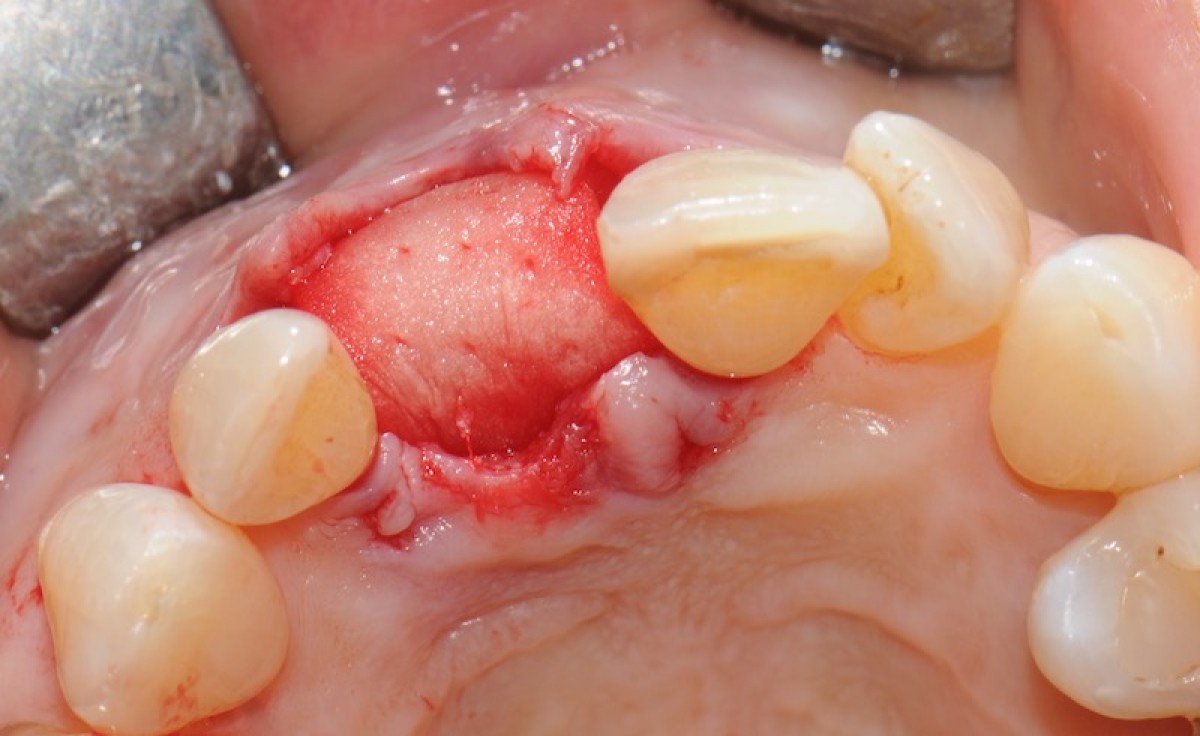
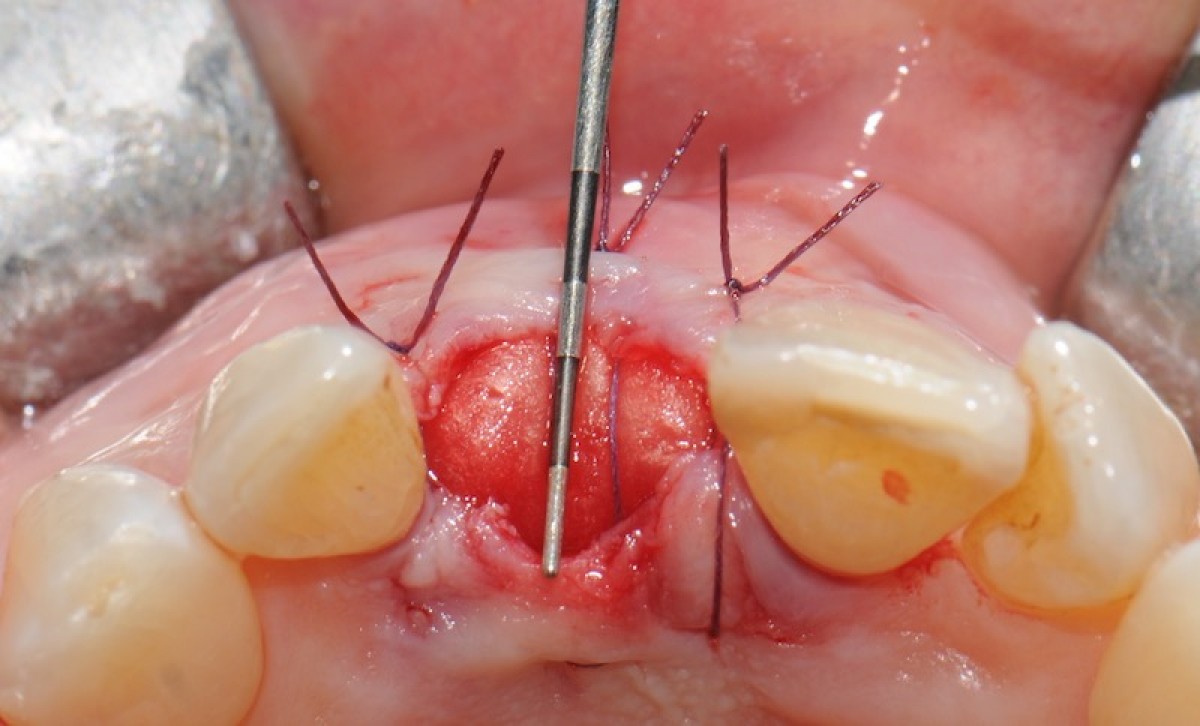
The objective of this prospective cohort study is to test the performance of a new xenogenic collagen matrix as a socket sealing material, to allow second-intention healing of post-extractive sockets filled with a xenogenic bone substitute or with an immediate submerged implant.
MATERIALS AND METHODS
10 patients were recruited, presenting a single-rooted tooth scheduled for extraction. After atraumatic tooth removal, the post-extractive alveolus received either a socket preservation procedure or an immediate submerged implant. In both cases, the gingival margins of the alveolus were sealed with a xenogenic collagen matrix (Mucoderm, Botiss Dental, Zossen, Germany). The following parameters were evaluated:
- exposed surface of the matrix at the end of surgery (T0);
- soft tissue healing at 1, 4, 6, and 8 weeks from surgery (T1-4);
- histological aspect of gingiva samples, harvested 20 weeks after surgery (T5);
- aesthetic performance provided by the socket sealing material (T4).
RESULTS
The results of the study showed that:
- the mean post-operative exposure area of the matrix was 26.25 mm2 (14.2 to 38.84 mm2 );
- 8 weeks after surgery, full wound closure was achieved in 9 out of 10 sites with healthy keratinized tissue;
- the histological evaluation of gingiva sample revealed the presence of healthy keratinized gingival tissue, with no signs of aberrations or anomalies;
- the mean colorimetric score ∆E between the regenerated site and the surrounding gingiva was 3.76 (3 to 6.55).
Seven out of 10 patients reported an excellent aesthetic integration of the matrix (∆E < 3.7).
CONCLUSIONS
Preliminary results from this study suggest that this new xenogenic porcine-derived collagen matrix could represent a valuable alternative to allow second intention healing of post-extractive sockets filled with a xenogenic bone substitute or with an immediate submerged implant. New randomized clinical trials are needed to confirm the preliminary results obtained in the study and evaluate the long-term benefits.
CLINICAL SIGNIFICANCE
The alveolar bone crest preservation techniques are used in clinical practice to reduce the volumetric bone contraction that occurs as a result of the avulsion of a dental element and, at the same time, to restore the correct profile of hard and soft tissues. In the present study, the use of the xenogenic matrix in collagen, in the coverage of a post-extraction site, seem to allow a correct regeneration and integration of the keratinized gingival tissue overlying the alveolus, both from a biological and an aesthetic point of view. However, the lack of consolidated scientific evidence regarding this technique requires the execution of new randomized clinical trials, aimed at confirming the results obtained, evaluating their long-term benefits.
For additional information:
Dental Cadmos n° 05/2018 - https://doi.org/10.19256/d.cadmos.05.2018.06
 Related articles
Related articles
Antibiotic prophylaxis (AP) still represents a common but often misused procedure in dental practice, thus aggravating the risk for antimicrobial resistance and adverse effects occurrence.
Oral surgery 27 October 2025
The authors assessed the incidence of postoperative bleeding in patients who were highly anticoagulated and in patients who underwent extensive oral surgical procedures and who continued using oral...
Implantology 02 October 2025
Proper implant treatment planning remains the first priority for implant success. Dental imaging is an important tool to accomplish this task.
Oral surgery 05 September 2025
Fentanyl, a short-acting synthetic opioid, has a pharmacokinetic profile suited to fast relief of brief episodic pain.
Oral surgery 22 August 2025
Thiel embalming technique: a valuable method for teaching oral surgery and implantology
Because of its high requirements on surgical experience and the need of complete understanding of the anatomy, oral surgery and especially implantology belong to the most demanding procedures in...
 Read more
Read more
News 27 February 2026
Align Partners Capital Management Inc. (“Align Partners”), a shareholder of Dentium Co., Ltd. (“Dentium” or the “Company”), has submitted formal shareholder proposals for inclusion in the...
News 27 February 2026
Angelalign Technology Inc. (6699.HK) (“Angel”) said a ruling by the Unified Patent Court of Düsseldorf, Germany, that it preliminarily cease its use of certain software functions that...
Prosthodontics 27 February 2026
Prosthetic implant rehabilitation using the scan-analog protocol: a clinical case
A digital workflow for prosthetic implant rehabilitation can start either from intraoral scans or from the scan of the patient cast models. However, the possibility of scanning oral impressions is...
Editorials 27 February 2026
Texas A&M College of Dentistry recently entered into an agreement with Shear Kershman Laboratories and medical device company Innovative MedTech Inc. to study BioViscid, a pharmaceutical delivery...
News 27 February 2026